Inappetence (also called hyporexia, with anorexia reserved for complete absence of appetite) is both a common presenting sign in cats visiting the veterinary clinic (Delaney, 2006) and a problem which frequently develops during hospitalisation, for example, post surgery (Chan, 2009). It is important because suboptimal nutrition can have negative effects on feline health and welfare via the multiple physiological consequences affected patients develop. Such effects include reduced immune function, slow wound healing, hepatic lipidosis and even shortened survival from a variety of illnesses (Chan, 2009). Management of inappetence can be challenging, as the cause may be multifactorial and complicated by stress, pain and adverse effects of medication. Therefore, in 2022, the International Society of Feline Medicine produced guidelines on the management of the inappetent hospitalised cat (Taylor et al, 2022a). Much of the information in the guidelines can also be extrapolated to outpatients, as it is important not to neglect the nutrition of any animals under veterinary care. Caregivers should also be educated on the importance of noticing and acting on inappetence. This article discusses some of the key points and recommendations in these guidelines. The guidelines are accompanied by supplementary materials, including feeding tube videos and documents containing information for caregivers.
Why is inappetence important in this species?
Cats have some unique nutritional requirements that differ from dogs, and these peculiarities relate to their origins as hunters, but also render them vulnerable to the negative effects of undernutrition (Figure 1). For example, cats have higher protein requirements than dogs and humans (Rogers et al, 1977), and a lack of enzymatic adaptation to reduced protein intake can result in lean muscle catabolism (Rogers et al, 1977). They also have requirements for other nutrients they cannot synthesise (for example taurine, arginine, fat-soluble vitamins and many minerals (Morris, 2002)), and failure to meet these, as well as energy requirements, is detrimental to the cat. Additionally, the impacts of inappetence are potentially greater in patients with underlying disease. So-called ‘stressed starvation’ describes inappetence plus a hypermetabolic state induced by inflammatory mediators and sympathetic nervous system stimulation caused by illness (Center et al, 2011). Hence, the impact of inappetence is even greater in sick cats, and both the undernutrition and the primary disease process should be addressed – in most cases, simultaneously.

Causes of inappetence
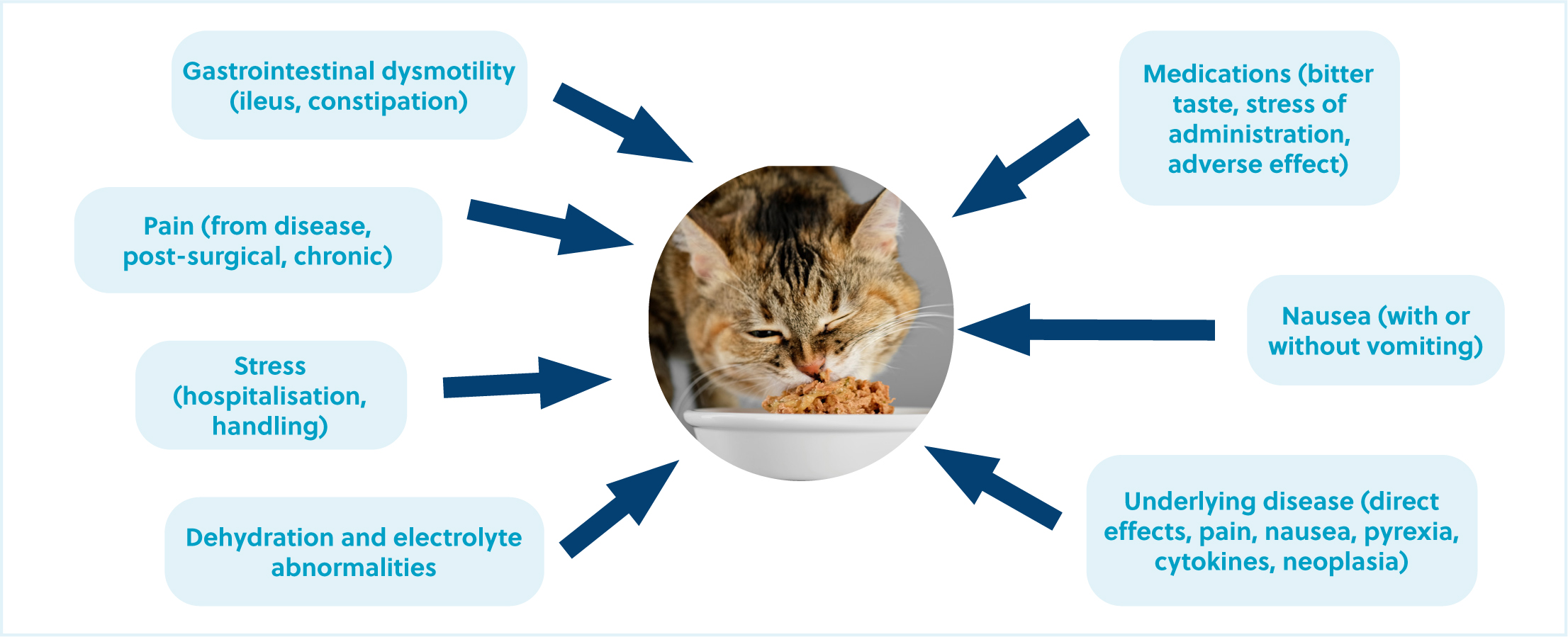
There are many reasons cats become inappetent, not just the underlying disease. In the hospital setting, many other factors can influence appetite (Box 1). In general, the most common causes of inappetence in cats are conditions causing nausea, pain or ileus, and additionally the effect of stress from hospitalisation will reduce voluntary food intake (Chan, 2009; Rodan and Cannon, 2016). In many cases there are several factors contributing to a reduction or loss of appetite, and all must be addressed to improve nutrition (Figure 2). Common diseases presenting with inappetence include conditions resulting in pyrexia (inflammatory, infectious disease), gastrointestinal and extraintestinal organ disease (pancreatitis, liver disease), respiratory and cardiac disease, urinary tract disease (upper or lower), neoplasia, chronic pain (for example, as a result of osteoarthritis) and neurological disease (Johannes and Musser, 2019; Chan, 2020). In addition to management of underlying disease, the treatment of nausea, pain, gastrointestinal dysmotility (constipation and ileus) and appropriate correction of fluid deficits and electrolyte abnormalities may improve food intake (Batchelor et al, 2013; Hill, 2019).
Box 1.Can medications themselves cause inappetence?Medications can have several effects on appetite. Many affect appetite directly (antibiotics, antifungals, opioids, non-steroidal anti-inflammatory drugs, chemotherapeutics, gastroprotectants, other drugs (methimazole, fluoxetine, mycophenolate, ciclosporin)) (Plumb, 2018), but also via bitter tastes (metronidazole, gabapentin, fluoxetine) and/or the stress associated with medicating orally. Medications given to cats in the hospital and before hospitalisation should be reviewed, and consideration given to withdrawing non-essential medications, giving oral drugs parenterally if appropriate and pain scoring to avoid excessive opioid use (Steagall et al, 2022).
Another significant cause of inappetence can be type of food offered during hospitalisation. Feline food preferences are set at an early age and may result in neophobia (dislike of novel tastes and textures) (Zoran and Buffington, 2011). Hence, failure to take a dietary history and offering unfamiliar, novel foods (including prescription diets) can result in reduced food intake. The International Society of Feline Medicine guidelines suggest that prescription diets for disease conditions should not be offered during hospitalisation as at best they may be refused, and at worst may result in longer term aversion to the chosen diet. Instead, in most cases, it is appropriate to offer small volumes of the cat's normal food to encourage food intake and caregivers can be asked to provide the familiar diet to encourage eating.
Reducing stress for hospitalised patients
Ideally, hospitalised cats will have an adequate voluntary food intake (Box 2). However, simply the novel environment with its sights, sounds and smells can reduce appetite. Many cats do not cope well with change and loss of familiar territory (Taylor et al, 2022b) and the veterinary clinic can be particularly challenging, with emotional and physical distress occurring in tandem. Providing a cat-friendly environment is vital to optimise nutrition and is outlined in the 2022 International Society of Feline Medicine and American Association of Feline Practitioners cat-friendly environment guidelines (Taylor et al, 2022b). The following should be considered:
- Providing a place to hide (and preferably perch) (Figure 3)
- Avoid mixing species in the ward
- Keep the ward quiet, although low-volume music can be played
- Use gentle interactions and avoid any heavy restraint (see Rodan et al (2022) for detail on cat-friendly interactions)
- Provide food so the cat can both access and move away from it, removing uneaten food
- Choose low-sided, ceramic bowls
- Avoid any coercing, wiping food on the cat or syringe or force feeding.
Box 2.Do you know how much your hospitalised cats should be eating (and how much they are)?All hospitalised cats should have their resting energy requirements calculated to avoid under- or over-feeding. Resting energy requirements should be calculated according to current weight even if the cat is over- or underweight, and correction of body condition is addressed once recovered.
- Resting energy requirement is calculated using 70 x bodyweight (kg)0.75
Bodyweight should be recorded at least every 24 hours and total calories adjusted by a maximum of 10% every 48–72 hours according to weight gain or loss. Food, both offered and uneaten, should be weighed and calories calculated (a laminated chart of calories per gram of commonly fed diets in the clinic kitchen is helpful) to allow documentation of the proportion of resting energy requirements consumed each day. This allows rapid identification of those consuming less than their resting energy requirement and requiring intervention. Hospitalisation record forms should include space for daily recording of food intake and the International Society of Feline Medicine guidelines include a feeding tube record chart to download.

Maximising positive experiences can improve a cat's emotional state and encourage voluntary food intake, so all opportunities should be taken to learn the cat's preferred interactions from the caregiver (for example stroking, being brushed) and quiet words and reassurance should be offered according to the cat's preferences. For additional information on the Cat Friendly Clinic scheme visit: www.catfriendlyclinic.org.
Nutritional assessment
Nutritional status should be measured in all patients and is considered the fifth vital assessment (after temperature, pulse, respiration and pain assessment) (Freeman, 2011; Chan, 2020). This assessment is particularly important in critically ill and hospitalised patients in order to identify those in need of nutritional support. The assessment involves taking a nutritional history, assessing body and muscle condition score, documenting risk factors for malnutrition such as severe vomiting and diarrhoea, prolonged inappetence and hypoalbuminaemia (Table 1). Patients are allocated a ‘risk’ level and feeding tubes considered for those with two or more high-risk factors. Performing this assessment daily has the benefit of facilitating prompt intervention when needed and should be repeated during hospitalisation as patient status can change.
Table 1. Assessment tool to identify the need for nutritional support
| Parameter | Low risk | Moderate risk | High risk |
|---|---|---|---|
| Food intake <80% RER for <3 days | ✓ | ||
| Food intake <80% RER for <3-5 days | ✓ | ||
| Food intake <80% RER for >5 days | ✓ | ||
| Presence of weight loss | ✓ | ||
| Severe vomiting or diarrhoea | ✓ | ||
| Body condition score <4/9 | ✓ | ||
| Muscle condition score: moderate to severe muscle loss | ✓ | ||
| Muscle condition score: mild muscle loss | ✓ | ||
| Hypoalbuminaemia | ✓ | ||
| Expected course of illness <2 days | ✓ | ||
| Expected course of illness 2-3 days | ✓ | ||
| Expected course of illness <3 days | ✓ |
A patient with two or more risk factors present should receive nutritional support immediately once stabilised. Patients with fewer than two risk factors should be closely monitored and reassessed daily.
RER: resting energy requirements
Modified from Perea (2015), with permission of Wiley-Blackwell, courtesy of the International Society of Feline Medicine and Taylor et al (2022a).
Appetite stimulants
Appetite stimulants can be helpful for both in- and outpatient management of inappetence, to increase caloric intake and try to prevent further undernutrition. Appetite stimulants should only be considered when conditions affecting appetite have been managed as much as possible (such as when the primary disease has been treated or is under treatment, nausea, pain, dehydration, ileus managed). Outside of these situations, the International Society of Feline Medicine guidelines suggest that they are likely to be ineffective. Prompt use (for example during the diagnostic work up or when managing more chronic undernutrition) may be beneficial.
Both mirtazapine (Mirataz, Dechra) and capromorelin (Elura; Elanco, USA) have been approved for use in cats (Wofford et al, 2018; Poole et al, 2019). The former is a transdermal preparation with the advantage of reducing oral medications. Transdermal mirtazapine has been shown to improve body condition score and result in weight gain in cats with various conditions (Quimby and Lunn, 2013; Poole et al, 2019) with minimal adverse effects. The effect of appetite stimulants should be closely monitored to avoid underfeeding and delays in more direct means of nutritional support such as feeding tubes. Commonly, the hospitalised patient is sent home with appetite stimulant therapy to ease the transition to the home environment and promote caloric intake during the recovery period.
Feeding tubes
Feeding tubes should be considered based on nutritional assessment and are indicated for patients consuming less than 80% resting energy requirement for 3 days or more (Freitag et al, 2000), those physically unable to eat (such as those with a jaw fracture), when undernutrition is predicted (for example post surgery) or when a patient is severely malnourished. They can also be useful for facilitation of medication compliance, particularly if prolonged courses of drugs are required (for example in the case of mycobacteriosis) and maintaining hydration. Before implementing a feeding plan via a tube, cats should have been rehydrated and be cardiovascularly stable with correction of electrolyte and acid-base abnormalities underway. Nausea, vomiting, pain and ileus should be managed alongside the feeding plan. Patient condition may affect choice of tube, but naso-oesophageal, naso-gastric and oesophagostomy tubes are the most frequently placed according to the International Society of Feline Medicine guidelines. Gastrostomy tubes may be needed for cats with oesophageal disease, for example. All tubes have advantages and disadvantages (Table 2) and the decision on which tube to place will depend on the individual patient.
Table 2. Advantages and disadvantages of commonly used feeding tubes
| Feeding tube type | Advantages | Disadvantages | Contraindications |
|---|---|---|---|
| Naso-oesophageal/naso-gastric |
|
|
|
| Oesophagostomy |
|
|
|
| Gastrostomy (placed surgically or percutaneously) |
|
|
|
Naso-oesophageal or naso-gastric feeding tubes
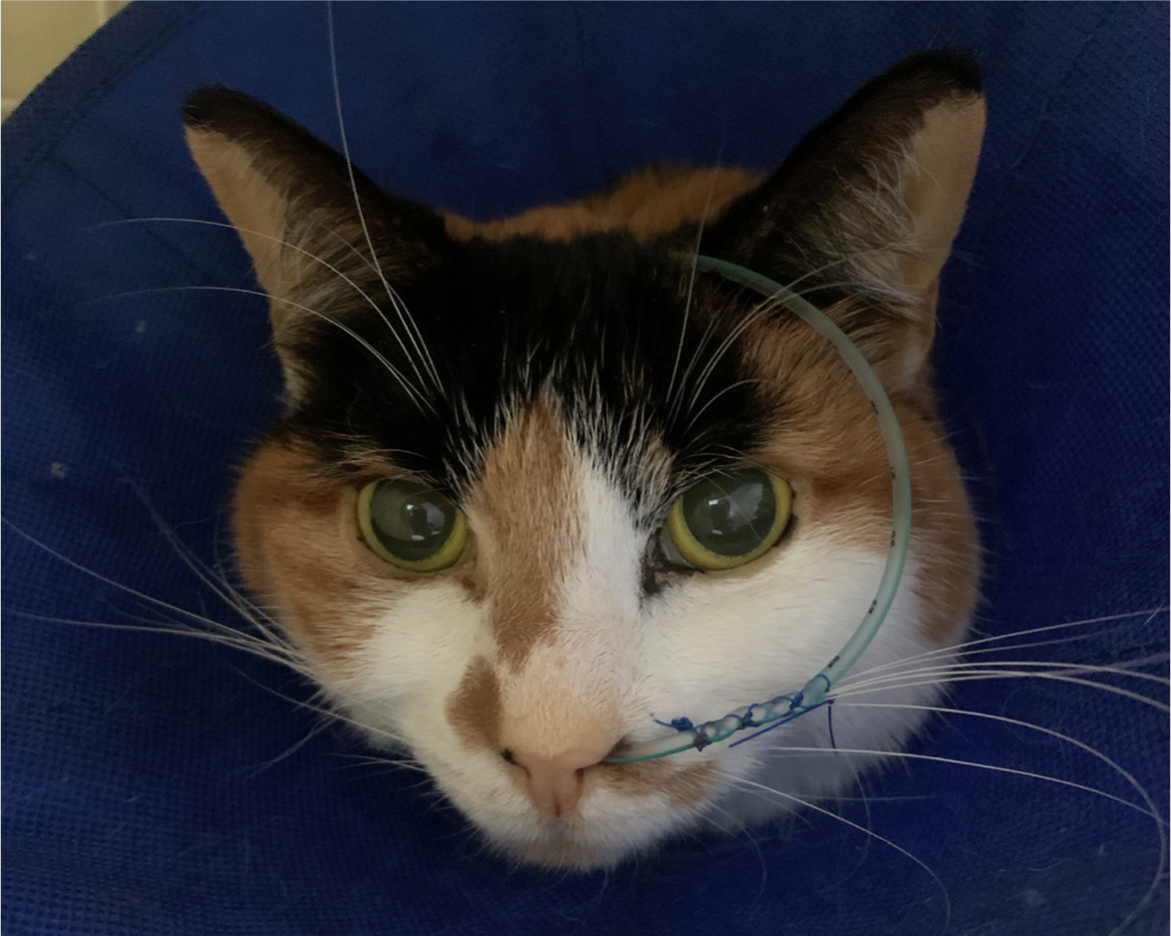
Naso-oesophagael or naso-gastric feeding tubes are suitable for short-term feeding (generally less than 5 days) in the hospital and can be placed in placed in sicker patients that are not stable for general anaesthesia to place a longer-term tube (Perea, 2015). Naso-oesophageal and naso-gastric tubes tend to be narrow bore, which limits diet choice and non-liquid medications will not pass through them. Although generally well tolerated, for some cats the presence of the tube can deter voluntary intake and they need to be removed to ‘test’ appetite. There seems to be no difference in complications between naso-oesophageal and naso-gastric tubes (Camacho and Humm, 2021), with naso-gastric tubes having the advantage of the opportunity to remove excessive gastric content in cats with ileus (Camacho and Humm, 2021). Gentle, cat-friendly handling and light sedation (such as with gabapentin or butorphanol), if required, can reduce stress while placing the tube in conscious patients (a video of naso-oesophageal and naso-gastric tube placement and use accompanies the International Society of Feline Medicine guidelines). Inadvertent tracheal intubation with resultant pneumonia is a major complication of naso-gastric and naso-oesophageal tubes but can be avoided by checking the tube placement before every use (Gajanayake, 2015) (Box 3). Other complications include dislodgement from patient interference and tube blockage (Gajanayake, 2015). The former can be prevented with a soft fabric Elizabethan collar (Figure 4) and cat-friendly handling, and the latter by flushing well and avoiding administration of crushed medications or thick foods.
Box 3.Checking tube positionThe feeding tube position should be checked after initial placement and before every feed. Dislodgement between feeds may occur, for example with vomiting or patient interference. A number of methods are used:
- Initial placement should be checked using radiography, fluoroscopy or endoscopy (consciously placed naso-oesophageal or naso-gastric tubes may not be checked with imaging if restraint causes stress, but must be checked in other ways)
- With a clean syringe, aspirate from the tube and check for negative pressure (naso-oesophagel and oesophagostomy tubes) or acidic gastric content (naso-gastric or gastrostomy tubes)
- Inject 5 ml air and auscultate the stomach for borborygmi (all tubes)
- Inject 2 ml sterile saline and observe for cough or respiratory signs (naso-oesophageal, naso-gastric and oesophagostomy tubes)
- Or, connect a capnograph to tube and check no reading for carbon dioxide (all tube types).
Oesophagostomy feeding tubes
Oesophagostomy tubes are a useful way of providing nutrition with the advantages of a larger bore, which facilitates various diets (including blended solid foods) and administration of crushed medications. They also provide the opportunity to leave in situ long-term for caregivers to use at home. Disadvantages include the need for anaesthesia for placement, management of a stoma and the need for a neck dressing (Perea, 2015), although fabric collars are generally well tolerated (Figure 5). Opportunities should be taken to place oesophagostomy tubes when inappetence is predicted or the underlying cause is being treated, for example when anaesthetised for imaging or surgery (a video of oesophagostomy tube placement and care accompanies the International Society of Feline Medicine Guidelines). The most common complications are stoma site infections and tube dislodgement (Nathanson et al, 2019), the former being more frequent in cats receiving glucocorticoids or chemotherapeutics (Breheny et al, 2019). In most cases stoma site infections can be managed with increased frequency of cleaning with antiseptics and application of topical antibiotics. Stoma sites should be checked and re-dressed at least once a day. Less common complications include haemorrhage and vagosympathetic trunk damage causing Horner's syndrome (this generally resolves spontaneously) (Warren et al, 2019).

Cats with any feeding tube should be offered food (unless contraindicated) before a feed and volume fed via tube reduced accordingly. Tubes should not be removed until voluntary intake is 75–100% of the animals resting energy requirements for at least 3–5 days.
What to feed
Choice of diet will depend on the individual case, and with naso-oesophageal and naso-gastric tubes is limited to liquid diets. Patients requiring protein restriction (such as those with advanced chronic kidney disease or hepatic encephalopathy) can be fed a renal liquid diet. Typically, recovery diets or convalescence diets are appropriate for most sick cats with feeding tubes as they are high in protein and energy dense (Chan, 2020). Most diets can be liquidised or blended into slurries to pass down oesophagostomy tubes or gastronomy tubes. All food should be warmed to body temperature and mixed well before being fed. To avoid obstruction, all tubes should be flushed with body temperature water before and after use.
How much and how often to feed via tube
The aim of nutritional support is not to correct body condition, but to stabilise the patient. For most cats, feeding one-third of their resting energy requirements on day 1, two-thirds on day 2 and reaching resting energy requirements on day 3 is appropriate (Chan, 2020). However, in patients with chronically reduced food intake, metabolic negative consequences and re-feeding syndrome are risks and a more conservative increase in food volumes over several days may be required. Adjustments can be made later to feeding amounts according to response and body weight. Growing kittens or those with high energy requirements (large exudative wounds or burns) may have requirements significantly exceeding resting energy requirements (Birkbeck et al, 2020; Chan, 2020).
Most sick cats benefit from smaller but frequent tube feeding (for example 3–6 meals a day (Chan, 2009)). The volume of each feed should be adjusted according to tolerance and given slowly, over a minimum of 10–15 minutes and generally of a volume between 5–15 ml/kg of bodyweight once full resting energy requirement is tolerated. Cats with gastrointestinal dysmotility may need smaller more frequent meals and even feeding via continuous rate infusion (rate 3–8 ml/kg/hr) (Chan, 2020). Cats should be fed slowly and be monitored for signs of nausea or discomfort (lip licking or backing away) and ideally have their head elevated and be sitting or lying comfortably. Feeding should not be rushed, but kept calm and without heavy restraint, providing the cat with reassurance.
Conclusions
Inappetence is an important clinical sign and undernutrition may have significant negative consequences in this species. Along with the primary disease process, there may be many contributing factors to consider and manage, including pain, stress and nausea. Prompt intervention, with appetite stimulants and feeding tubes if required, may optimise recovery from many conditions. The 2022 International Society of Feline Medicine guidelines on the management of the inappetent hospitalised cat provide practical information on this challenging problem and detailed guidance on tube placement and management.
KEY POINTS
- Inappetence should be addressed in feline patients to prevent negative consequences of undernutrition, including reduced wound healing, immune dysfunction, hepatic lipidosis and reduced survival.
- Causes of inappetence may be multifactorial and include stress in hospitalised patients.
- Pain, nausea, ileus, fluid and electrolyte abnormalities should be addressed to promote voluntary food intake.
- Appetite stimulants used judiciously alongside investigation and treatment of the underlying disease may improve nutrition.
- Feeding tubes should be considered in patients with chronic undernutrition, predicted inappetence and those in poor body condition. They can also be useful for medicating and providing fluid.


